Introduction
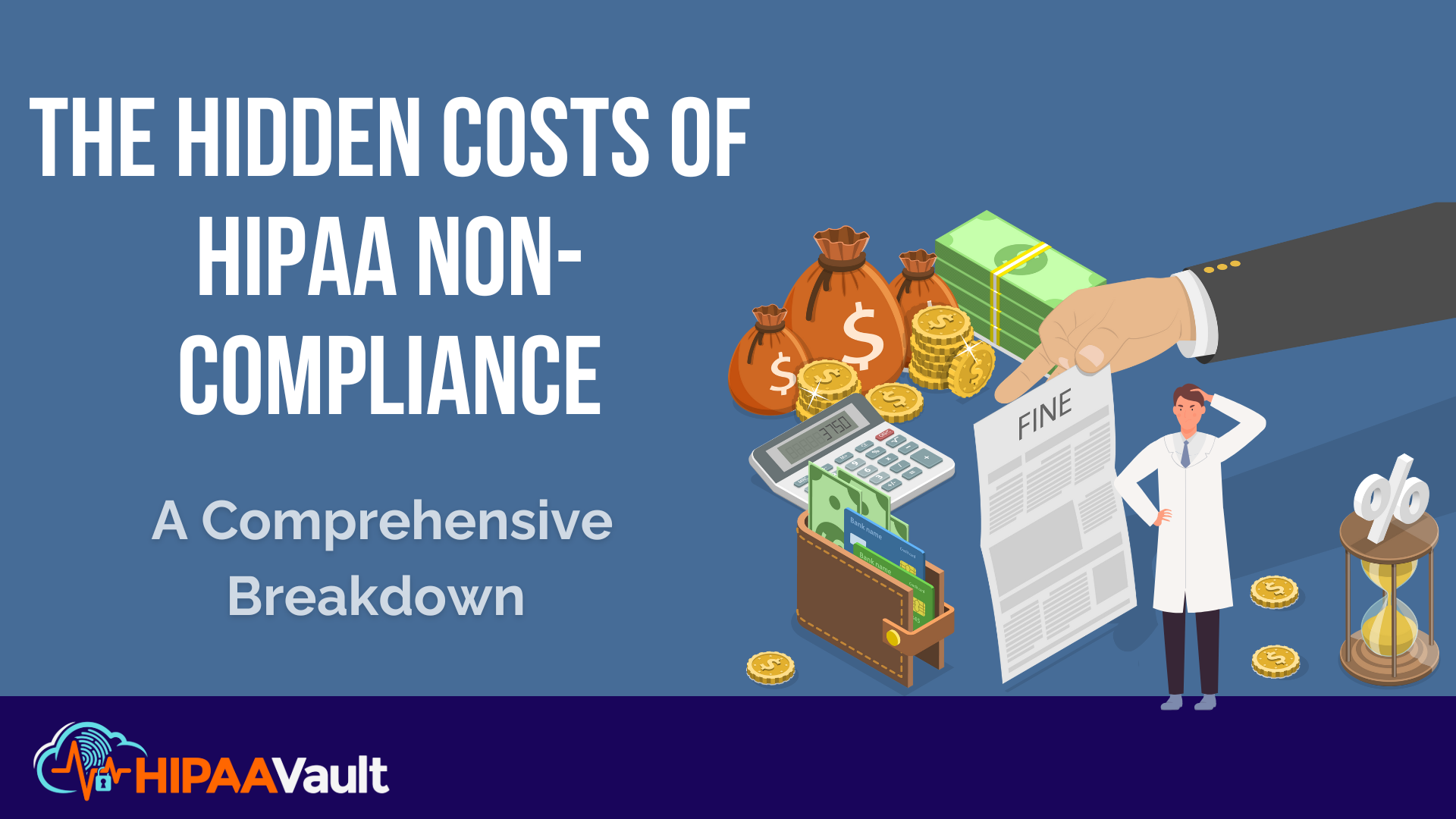
Cybersecurity breaches in the healthcare industry have reached an alarming rate, costing organizations over $10 billion annually. Despite this staggering statistic, many healthcare providers and business associates continue to underestimate the far-reaching consequences of HIPAA non-compliance. Failing to implement the necessary safeguards to protect electronic protected health information (ePHI) not only invites hefty fines but also puts patient trust, business operations, and legal standing at risk.
Ensuring HIPAA compliance is not merely a matter of regulatory adherence — it is a crucial component of a well-functioning healthcare organization. In this comprehensive breakdown, we will explore the various hidden costs of HIPAA non-compliance and provide actionable strategies to help your organization strengthen its security posture while maintaining compliance.
Understanding HIPAA Compliance Requirements
The Health Insurance Portability and Accountability Act (HIPAA) was designed to establish clear guidelines for the secure handling of patient data. To fully understand the implications of non-compliance, organizations must familiarize themselves with the core rules of HIPAA:
- HIPAA Privacy Rule — Dictates how patient data should be collected, stored, and shared while ensuring individuals’ rights to access their health information.
- HIPAA Security Rule — Requires healthcare entities to implement administrative, technical, and physical safeguards to protect ePHI from unauthorized access or breaches.
- HIPAA Breach Notification Rule — Mandates that covered entities notify affected individuals, HHS, and sometimes the media when a data breach occurs.
Failure to comply with these provisions not only exposes organizations to financial repercussions but can also have long-term operational and reputational consequences that are often underestimated.
1. Financial Penalties for Non-Compliance
One of the most immediate and visible costs of HIPAA non-compliance is financial penalties. The Department of Health and Human Services (HHS) Office for Civil Rights (OCR) enforces these fines based on the severity and nature of the violation. The penalties are structured into tiers based on culpability:
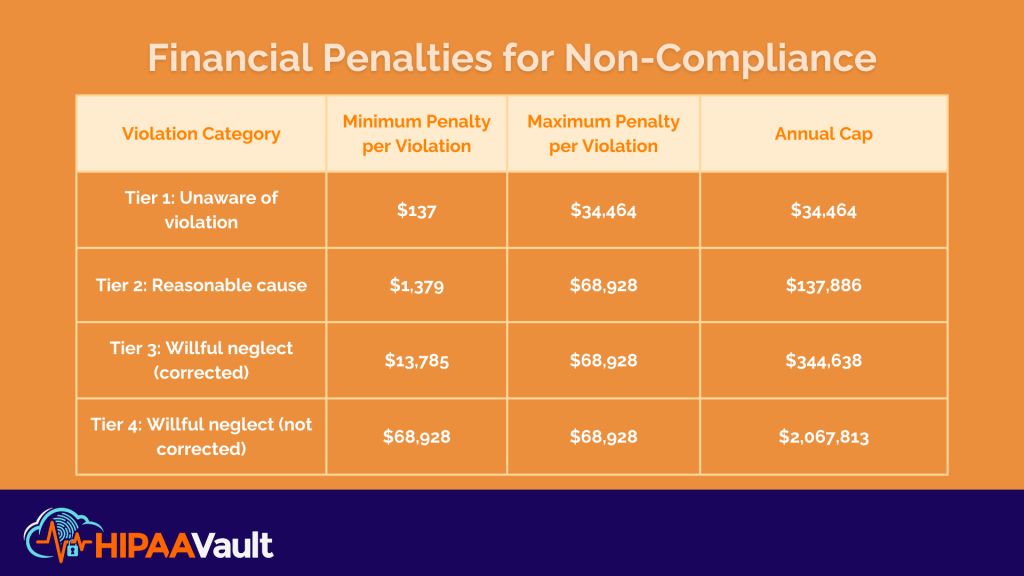
The financial impact of these fines can be devastating, particularly for smaller healthcare organizations that operate on tighter budgets. Moreover, these penalties do not account for additional costs related to breach mitigation, security upgrades, and potential class-action lawsuits that may arise from affected patients.
Real-World Example:
In 2020, Premera Blue Cross, one of the largest health insurers in the U.S., was fined $6.85 million for failing to implement proper security protocols. This breach resulted in the exposure of 10.4 million patient records, causing long-term reputational damage and legal repercussions that extended beyond the immediate fine. It’s important to note that HIPAA violations often result in settlements exceeding standard fine caps due to additional legal claims and mitigation costs.
How to Avoid These Costs:
To prevent financial penalties and compliance gaps, organizations should proactively:
- Conduct regular HIPAA risk assessments to identify vulnerabilities.
- Implement strong encryption measures to safeguard ePHI.
- Partner with a HIPAA-compliant cloud hosting provider like HIPAA Vault for secure data management and compliance assistance.
2. Reputational Damage and Loss of Patient Trust
Beyond financial penalties, a HIPAA violation can cause irreversible harm to an organization’s reputation. Patients trust healthcare providers to protect their sensitive information, and a breach can lead to significant fallout, including:
- Decreased patient confidence in the organization’s ability to handle sensitive data.
- Negative press coverage that can damage brand perception and credibility.
- Increased patient churn, forcing healthcare providers to invest heavily in reputation recovery campaigns.
Case Study:
In 2015, Anthem Inc., one of the largest health insurers in the U.S., suffered a massive cyberattack that exposed the records of nearly 80 million individuals. This breach led to widespread distrust, costly litigation, and a record-breaking $16 million settlement with OCR. The damage to Anthem’s reputation was immense, and rebuilding patient trust required extensive efforts.
How to Maintain Patient Trust:
- Regularly train employees on HIPAA compliance best practices.
- Deploy secure hosting solutions that ensure ePHI protection.
- Establish incident response protocols to address breaches swiftly and transparently.
3. Operational Disruptions and Recovery Costs
The financial penalties and reputational damage caused by non-compliance are just the beginning — many organizations also face significant operational disruptions following a breach. The fallout from a security incident can result in:
- Extended system downtime, affecting patient care and administrative operations.
- Costly forensic investigations to determine the source and scope of the breach.
- Lengthy legal battles that consume time and resources.
Example:
A ransomware attack in 2021 forced a major hospital network to shut down its entire IT infrastructure. The attack caused weeks of operational delays, required costly forensic investigations, and ultimately led to over $50 million in damages, not including lost revenue from patient diversions and legal fees.
How to Prevent Disruptions:
- Establish a comprehensive incident response plan.
- Implement real-time security monitoring to detect and neutralize threats early.
- Use secure cloud hosting with robust disaster recovery capabilities, like those offered by HIPAA Vault.
Conclusion
HIPAA non-compliance carries far-reaching consequences that extend well beyond financial penalties. Organizations that fail to prioritize compliance risk not only costly fines but also damaged reputations, operational setbacks, and potential legal action. By taking a proactive approach to compliance, healthcare providers can avoid these pitfalls and build a more secure, trustworthy practice.
Investing in HIPAA-compliant security solutions is the best defense against these risks. Partnering with an experienced provider like HIPAA Vault ensures your organization benefits from 24/7 managed security, encrypted cloud hosting, and expert compliance support.
Don’t wait until a breach happens. Contact HIPAA Vault today to secure your healthcare data and maintain compliance.